We treat hemato-oncology diseases almost fully in accordance with Western standards. However, there are also challenges

Published Feb. 13, 2024 11:51
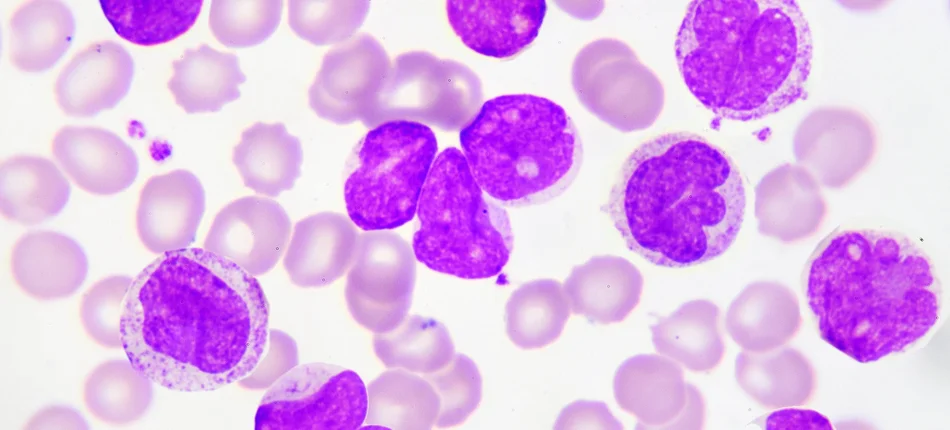
Although experts agree that in the care of patients struggling with hemato-oncologic diseases such as chronic lymphocytic leukemia and plasmocytic myeloma, we have a standard of treatment largely in line with Western standards, the results of treatment are still not entirely satisfactory. Data from the National Cancer Registry show that survival in Poland is still 10 percent lower than in Western European countries.
Meanwhile, we can talk about a breakthrough that has been made in the treatment of PBL. This is a therapy using two groups of drugs: Bruton's kinase inhibitors such as acalabrutinib, zanubrutinib and ibrutinib. All of these drugs are reimbursed in Poland. An alternative therapy is venetoclax in combination with obinutosumab, also reimbursed for first-line treatment.
- We are missing a single therapeutic regimen that combines two innovative drugs: ibrutinib and venetoclax. This is a very interesting regimen, because it combines two innovative drugs, and this therapy is interesting in that it is a time-limited therapy. Bruton's kinase inhibitor therapy lasts for many years. Most people will receive it over 5 years of life. In this case, by contrast, we have 15 months of treatment," pointed out Prof. Krzysztof Jamroziak of the Department of Hematology, Transplantation and Internal Medicine at Warsaw Medical University.
This is important primarily from the patient's point of view. The short duration of therapy and the oral form of administration mean that treatment does not involve frequent visits to health centers. There is also no risk of side effects that would be associated with intravenous administration. This also translates into systemic benefits. In the long run, such treatment not only generates savings, but also streamlines treatment and allows more patients to be cared for at the centers.
- The patient needs less care, that is, the treatment involves fewer hospital stays or clinic visits. This is a generally healthy patient who can function normally. So this is the kind of treatment that is most lacking. There are also minor deficiencies that can be easily corrected, such as expanding the indications for registered drugs such as Bruton's kinase inhibitors, for example. Their registration is limited to certain groups of patients either with high cytogenetic risk or diseases that do not qualify for intensive treatment. This could also be leveled for everyone, as one patient can only get one first-line therapy anyway, and this would help individualize the therapy and match it to the patient's profile, to potential side effects," Prof. Jamroziak pointed out.
A therapeutic model, which is the most urgent need in PBL, could be included in a group of up to 400 patients, according to clinicians.
Reimbursement needs are also related to the treatment of plasmocytic myeloma. The first regimen awaiting a reimbursement decision is the daratumumab, dexamethasone, carfilzomib regimen.
- This is a very important regimen for the treatment of relapsed patients, especially in the population of patients previously treated with lenalidomide. If we take into account that lenalidomide is a generic, widely available drug, which in principle is a key first-line treatment for all patients, for transplant patients and for transplant-ineligible patients, different therapeutic regimens will be used, usually two-drug or three-drug, depending on the risk burden. For most patients, it will be a three-drug regimen," pointed out Prof. Krzysztof Giannopoulos of the Department of Experimental Hematooncology at the Medical University of Lublin.
It is worth recalling that since January, the most effective first-line therapy regimen for patients ineligible for transplantation has already been reimbursed: daratumumab, lenalidomide and dexamethasone.
Another challenge for the future, according to the professor, is the reimbursement coverage of bispecific antibodies for the treatment of relapsed or refractory plasmocytic myeloma.
- Three of them are already registered in the world and in Europe, that is, also in Poland. These are taletamab, elranatamab, teclistimab. As far as I know, the latter is the most advanced in the reimbursement process," the professor pointed out.
The preparation that Prof. Christopher Giannopoulos discussed is an antibody that binds CD3 antigen on T lymphocytes and B cell maturation antigen (BCMA) on myeloma cells.
Mateusz Oczkowski, deputy director in the Department of Drug Policy and Pharmacy at the National Health Fund, addressed the reimbursement needs reported by clinicians. In his opinion, the combination of carfilzomib and daratumumab therapy in myeloma will be a major financial challenge. The reimbursement process thus promises to be tough.
- It is much easier when we have a drug combination in which the substance will have a generic equivalent in a while. That will be the case with pomalidomide this year. So new responsible parties will probably come, new biosimilar drugs will appear, and eventually it will end up in the chemotherapy catalog," he said.
- In the process, we also have the bispecific antibody teclistamab. It is already a drug that has been given the designation of "breakthrough therapy." Since it's a breakthrough therapy, we need to look into it," he admitted.
Matthew Oczkowski also addressed the need to reimburse ibrutinib in combination with venetoclax for first-line PBL treatment.
- This therapy is worth considering, and the minister will certainly engage in further discussions with the responsible party," he pointed out.















