Drug-resistant depression: not all patients who deserve it can benefit from drug program

Published July 9, 2024 11:35

Professor, I would like us to talk about patients being treated for drug-resistant depression. A drug program for this group of patients was launched last July. Can we already say what has happened over this past year?
This is a tremendous event for us, the psychiatric community nationwide, for the reason that it has brought the first drug program into our field that can finally offer patients with this thankless disease a therapeutic outlet. Patients with drug-resistant depression often do not respond to subsequent lines of treatment, the kind of standard therapeutic steps we take in treating any depression. And even combinations of different drugs don't transfer much, don't change their condition. They are often stuck in this suffering for months or even years. They are unable to get out of it on their own, they are often unable to function. And this mental pain they experience is often very great. Therefore, the emergence of an opportunity to offer these patients reimbursable therapy that would help them end this depressive state is a revelation for everyone, for patients and for us doctors.
Can we already say how many beneficiaries of this program there are?
As far as I know, there were dozens of patients qualified nationwide. How many of them are currently continuing this therapy is hard for me to say, because I don't know the current data. But more people are coming forward. Because undoubtedly, as estimates show, there are at least several to several thousand of these patients nationwide. These are people who suffer from depression that does not lend itself to treatment, that is, the kind of depression where you have to use some extraordinary method to end it.
What are the eligibility criteria for this program?
In addition to this diagnosis, in order for it to be recurrent depression, these should be people who have a personality disorder ruled out, have bipolar affective disorder ruled out; are not addicted and people in whom this depression is at least moderate or severe in terms of severity of symptoms. If this episode lasts for at least 6 months and there have been many antidepressants, antidepressant treatments tested, then we can invite this type of patient to the drug program.
It's probably quite a complicated process to explain in a few sentences, but what is the benefit of this innovative treatment?
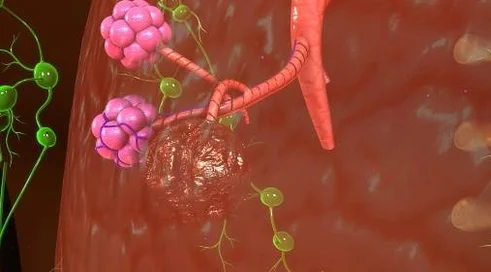
This new innovative treatment is a drug that has been known around the world for decades, but in a new form. First, the enantiomer, esketamine, is crafted so that it can be administered intranasally. And administered over several consecutive applications, it can already completely change the patient's condition, life and well-being, lying often in bed depressed patients start and restore normal functioning. What is important - the boon of this treatment is that it works through a completely different mechanism than all the traditional antidepressants we have on the market, which work mainly through the serotonergic and noradrenergic systems. Some of them also through the dopaminergic system. And esketamine works through the glutamatergic system, that most prevalent neurotransmitter system in the nervous system.
Do you think the program should change in any way so that maybe more patients can benefit from this therapy?
These few months (it will be 8 at the moment), as the program practically entered into clinical practice at the end of last year, it took several months of preparation and various legal documents enabling the program to be contracted at the National Health Fund, have shown us that these qualification and disqualification criteria are not precise enough to enable all patients who deserve this treatment to qualify for the program. In view of this, we are among the experts at the moment at the stage of revising these eligibility criteria of the drug program so that more of these patients can be qualified.