Modern treatment exists, but not for everyone. Patients with relapsed DLBCL are still waiting for new reimbursements and better diagnostics

Published Nov. 12, 2025 13:06
Professor, what are the characteristics of diffuse large B-cell lymphoma (DLBCL) and what are its symptoms?
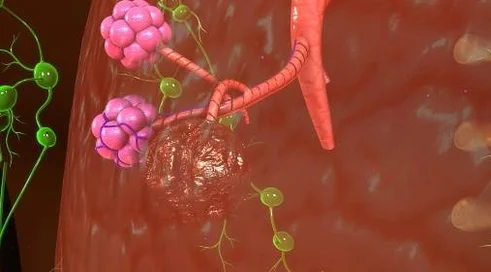
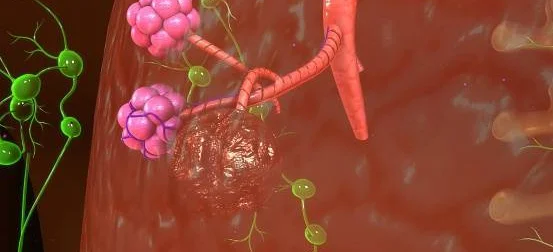
Diffuse large B-cell lymphoma DLBCL is an aggressive neoplasm of the lymphatic system that usually develops rapidly and usually results in local and often general clinical manifestations. Local symptoms are associated with the presence of lymphoma cells, usually in the form of a tumor. Such a tumor can compress vessels, nerves or even entire organs. Hence there may be pain or features of organ dysfunction, such as hydronephrosis or liver damage with jaundice. DLBCL can also cause systemic symptoms related to the proliferative activity of the lymphoma and the secretion of various substances, cytokines, which affect the functioning of the entire body. These symptoms include unexplained fevers usually occurring in the afternoons, weight loss and clammy night sweats, requiring a change of clothes. In addition, these symptoms may be accompanied by fatigue, which is a constant feeling of tiredness that does not subside after a night's rest.
DLBCL lymphoma can occur anywhere, so local symptoms can vary widely. Sometimes a patient comes to the family doctor, sometimes with a very trivial complaint, such as back pain, which is increasing and may initially be treated as a simple degenerative or inflammatory lesion, often seen in older people, and it is worth noting that DLBCL is also most common in older people. Sometimes younger patients also get the disease, but the median incidence is between the ages of 65 and 70. These patients may also have comorbidities and DLBCL can sometimes mimic the severity of the comorbidities. Sometimes DLBCL appears in the central nervous system, in which case the first symptom may be headaches, dizziness, sudden onset of epilepsy or visual disturbances. The spectrum of symptoms can vary greatly, and it is not always easy to suspect that lymphoma is the cause of these changes. It is extremely helpful to have imaging studies sometimes of the whole body, which can localize the cause of the complaints and localize the tumor infiltration, which always requires histopathological examination. Examination by fine-needle biopsy is not enough - if lymphoma is suspected, examination by thick-needle biopsy or, preferably, collection of the entire cancerous lesion is necessary, which makes it possible to find out what the cells are, identify whether they are lymphoma cells and, at the same time, determine what type of lymphoma it is. One of these more common types is precisely diffuse large B-cell lymphoma.
Professor, what is the prognosis for patients who already have this diagnosis? Is this a disease that can be cured?
Let's clarify what aggressive lymphoma means, because on the surface it can be disturbing news. Aggressive lymphoma means that it grows rapidly and therefore requires treatment. With sufficiently intensive therapy, a patient can be completely cured, unlike so-called indolent lymphomas, where the possibility of a permanent cure is still very limited, although usually indolent lymphoma is not life-threatening at the time of diagnosis.
In contrast, about 70% of patients with DLBCL lymphoma, and some say that with modern treatments nearly 80%, can be cured with first-line treatment. So, looking at lymphomas from this side, this is a cancer that heals relatively well.
There have been a lot of positive changes in the field of hematooncology in recent years. And what is the system of care for patients with this lymphoma and what treatment options are available in our country?
As for the system, there is an important issue: who should treat lymphoma patients. Formally, such patients can be treated by both clinical oncologists and hematologists. The treatment of lymphomas is specific, sometimes different from the treatment of solid tumors. Therefore, I believe, without disparaging clinical oncologists, that specialized treatment of DLBCL lymphoma should be carried out in a center with experience in treating this type of cancer, that is, in an onco-hematology center. This does not necessarily have to be a large academic center, but simply a good center that collaborates with a reference center on a daily basis. We are waiting for the development of a nationwide hematology network, where smaller hematology centers would be linked to reference centers, so that it is easy not only to determine the correct diagnosis, but also to determine the patient's treatment path. Whether this is a patient who can be treated successfully at a smaller center or should be treated at a reference center from the beginning. At the moment, access to different treatment options for patients who are diagnosed in cancer centers - especially the smaller ones - is unfortunately different than in onco-hematology centers. Typical oncology centers often don't have all the available treatments or don't have in-house experience with them.
In our unit, which is a large academic unit and would meet all the criteria of a referral center, if any lymphoma is suspected, the patient's path is relatively simple. The patient, having a DILO card, within 2-3 weeks has basic examinations to determine the risk of the disease, the stage of the disease, and a decision is made on the treatment. On the other hand, the problem is situations in which the patient is referred for diagnosis of presenting symptoms, but without the suspicion that their cause is lymphoma. In these situations, there may be a delay in making the diagnosis due to the prolonged time to biopsy and its evaluation by a pathomorphologist. The lack of a sufficient number of pathomorphologists specializing in the diagnosis of cancers of the lymphatic system is a weak point in the health care system in Poland. Cancers of the lymphatic system are plentiful, so a skilled experienced eye and diagnostic, cytochemical and molecular tests are essential to diagnose lymphoma patients in a modern way. There are ideas in some countries that lymphoma treatment centers should be certified in the sense that such certification would determine the capabilities, the minimum set of tests that a center should offer to a patient in order to correctly diagnose and correctly prescribe treatment. The creation of a hematology network, with the development of laboratories dedicated to the diagnosis of hemato-oncologic malignancies, could improve the current situation.
Something like breast cancer units?
Yes. In our center we are creating such a unit on lymphoma, but this is our local activity, while it does not have formalized statutory structures. It is not a requirement at all that a center treating lymphoma should have such an interdisciplinary team. If there were such a requirement, many problems would be solved, just as the DILO card solved many problems in access to oncology care. All this is overseen by the national consultant in hematology, Professor Ewa Lech-Marańda, who has an idea and knows how she would like to improve the system of care for patients with hematopoietic diseases, including those suffering from lymphomas. I want to emphasize that it is to the credit of many that we now have one of the best accessibility in Europe to modern treatments for lymphomas, including specifically large B-cell lymphoma. We actually have most of the drugs, including targeted drugs. We also have dual-specific antibodies available that use our immune system to fight the cancer. Finally, we have modified our own lymphocytes in the form of CAR-T therapies. These therapies in DLBCL lymphoma are available. All of this makes the treatment of DLBCL lymphoma state-of-the-art, and we believe that this will be evident in our country's cure rates in the near future.
What are the effects of bispecific antibodies and how can they help patients with relapsed and refractory DLBCL lymphoma?
Bispecific antibodies - a more appropriate name in Polish should be bispecific antibodies - are proteins that have domains on their two ends that bind to the cell at one end of the tumor, and at the other end to the active cells of the immune system - the T lymphocytes. This physical proximity of the T lymphocytes to the tumor cells causes activation of the T cells and triggers a cytotoxic reaction, so that the destruction of the tumor cells takes place. The cancer cells naturally defend themselves against the T cells, which they do not allow to reach their surface, making our immune system unable to fight the cancer. These antibodies break through the tumor's defenses, bringing the T lymphocytes closer to the cancer cells so that their destruction can occur. This treatment is also effective in patients who are resistant to standard chemotherapy. These antibodies were initially used as monotherapy without other drugs, but we now have breakthrough reports of using dual-specific antibodies with conventional chemotherapy as early as second-line treatment, i.e. in cases of lymphoma relapse or primary resistance, and in patients who do not qualify for other treatments such as autologous transplantation or even CAR lymphocyte therapy. The randomized Phase III STARGLO Global Phase III Trial (i.e., the study with the highest quality of clinical evidence) (NCT04408638), comparing the dual-specific antibody glofitamab administered with GemOx chemotherapy to standard second-line treatment i.e., a GemOx regimen with rituximab, showed an improved rate of up to 33% complete remission and significant improvements in overall survival and progression-free survival of 25,5 and 13.8 months, reducing the risk of death by 38% in patients receiving the dual-specific antibody with GemOx chemotherapy compared to standard GemOx treatment with rituximab. In conclusion, GemOx chemotherapy in combination with the dual-specific antibody glofitamab has shown remarkable efficacy, extending patients' survival not only by many months, but even years. Longer follow-up results suggest that about 40-45% of these patients are even cured after a short time-limited treatment of glofitamab with GemOx chemotherapy.Consequently, the latest recommendations of the European Hematology Association (EHA) and the European Society of Clinical Oncology (ESMO) for the treatment of DLBCL unequivocally recommend the Glofit-GemOx regimen, giving it the highest strength of recommendation (IA) in the 2nd line treatment of R/R DLBCL in patients ineligible for auto-HSCT and CAR-T.
We are waiting for reimbursement for this treatment modality. In addition to all the tools we have, we hope that this regimen, which is glofitamab with GemOx therapy, will also be available soon.