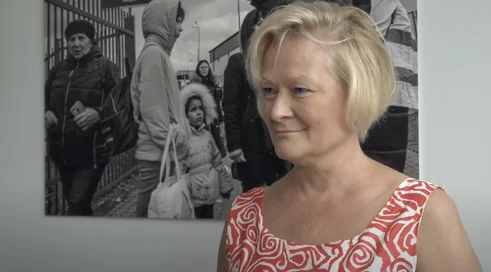
Prof. Agnieszka Wierzbowska: We are witnessing a major breakthrough

Published Feb. 13, 2024 08:00

What does new medicine offer today for patients with acute myeloid leukemia, but in slightly worse shape, older, with comorbidities, who are not eligible for chemotherapy or transplantation?
Over the past three years, treatment prospects have changed for this group of patients. Until now, it was thought that there was little we could do to help elderly patients who were not eligible for intensive treatment; we were trying to prolong overall survival and improve quality of life. One breakthrough was the introduction of hypomethylating drugs more than 10 years ago. Nevertheless, the most effective treatments still did not lead to satisfactory results. I am referring primarily to the relatively short overall survival time with a median of 7-8 months. A big step was the introduction of venetoclax in combination with azacitidine. This is a relatively universal treatment that has further extended median overall survival. I think we are now witnessing a major breakthrough, because for the treatment of elderly people ineligible for intensive treatment, we are beginning to introduce a personalized treatment strategy and use targeted therapies. It has been known for years that acute myeloid leukemia is not a homogeneous disease (it is genetically heterogeneous) and therefore one type of treatment is not always equally effective in different genetic subgroups. This strategy has found a place in the treatment of fit patients, i.e. those eligible for intensive chemotherapy or transplantation, in whom we conduct genetic screening and stratify patients for treatment with different drugs, depending on their genetic profile. And this strategy is just entering the population of elderly patients who are ineligible for intensive treatment. Here, a huge breakthrough is the registration of ivosidenib. It's a selective inhibitor of the isocitrate dehydrogenase IDH1, a mutation of which is found in about 10-12 percent of acute myeloid leukemia patients. And it turns out that the introduction of such a targeted treatment (the inhibitor inhibits the function of the mutated, abnormal enzyme in leukemic cells in combination with standard chemotherapy, the mainstay we've been using for years, azacitidine) is yielding spectacular results. The median overall survival in this group of patients reaches about 30 months (that's nearly 2.5 years). I think this is the best result of median overall survival that has been achieved so far with various non-intensive treatment options. This clearly shows that it is the personalized approach to patients treated with low-dose chemotherapy that makes sense and translates into better treatment outcomes.
Also for a better quality of life?
Undoubtedly, yes. The results of the AGILE trial, which was a registration study of ivosidenib, confirmed unequivocally that patients treated with ivosidenib in combination with azacitidine have better quality of life in all elements and tests verifying quality of life, compared to patients treated with standard azacitidine. I think it is also worth emphasizing that the combination of azacitidine with ivosidenib is a complementary treatment. The two drugs have a synergistic effect, but the benefit to patients (important for this patient population) is a reduction in infection rates. That is, the severe infectious complications (pneumonia, severe infections) that often lead to patient deaths in this population are less frequent. This is probably due to the fact that ivosidenib accelerates the differentiation of blast cells into normal, mature granulocytes, so that immune reconstitution occurs sooner during the treatment process, which of course also has a protective role in protecting against various infectious complications.
The AGILE study ended for an unusual reason....
Yes, it's true. The AGILE trial - a rarity in trials in acute myeloid leukemia - was terminated prematurely, that is, before the target number of patients in the trial had been reached, because of the very good treatment results in the study arm. The study's safety monitoring committee, after an initial evaluation of the randomization of seventy-some patients to each arm, decided to terminate the trial and proceed to registration, on the grounds that the benefit enjoyed by patients in the study arm was so great that it would not be ethical to continue the trial and recommend azacitidine monotherapy to patients with the IDH1 mutation.
Finally, I will ask about reimbursement priorities in 2024?
In acute myeloid leukemia, we have been in a very comfortable position over the past year, having most of the drugs registered in the world at our disposal. We were able to treat patients as we do in Europe. On the other hand, the registration of ivosidenib, which took place last May, presents us with new challenges. And this is the reimbursement priority at the moment for acute myeloid leukemia patients who are not eligible for intensive chemotherapy. This challenge facing us, the payer, will not be so terrible, because this treatment affects a relatively small number of patients. Nationally, the number, I think, will not exceed 100. Therefore, I hope that the reimbursement process will go very smoothly.