Iwona Schymalla: Is PPH a major challenge for perinatal care in Poland?
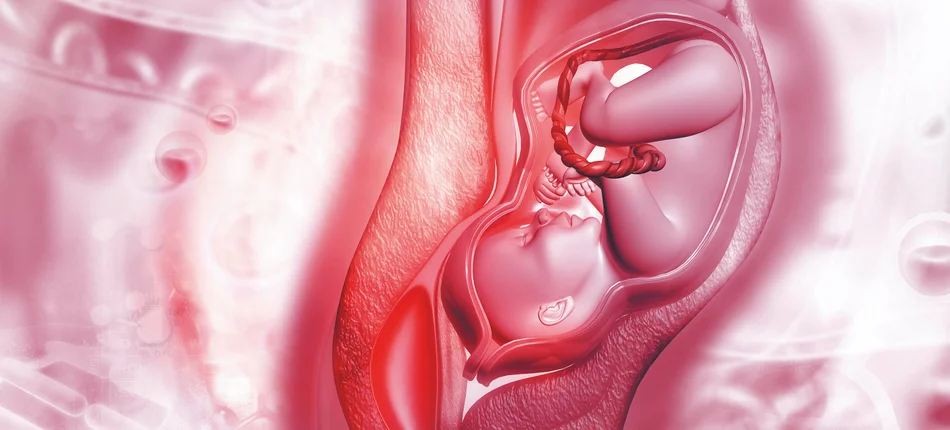
Maciej Socha: PPH is indeed a major perinatal care issue as it poses a huge risk for both the mother and the baby. It is particularly worrying when we have a healthy patient who is bound to deliver without any complications and still statistically 5 up to 10 deliveries will feature considerable blood loss. Considerable blood loss defined as hemorrhage is classified as perinatal issue which we can manage quite well- we are equipped with relevant preventive tools. However, it has to be stressed that such a situation can easily trigger a cascade of medical conditions that can result in the patient's death.
Iwona Schymalla: There is one more alarming situation when we think about COVID-19 epidemic. Namely, OBGYN wards require substile amount of blood for transfusions. The question is if it is available?
Maciej Socha: OBGYN wards have always been in demand for blood as you mentioned. Blood transfusion is a preventive method as the cascade of events that can occur during labor is largely dynamic and can lead to the patient's death. The assumption is that if the patient dies during labor, it was probably caused by PPH. Therefore, it is absolutely essential to secure sufficient stocks of blood for transfusion. Unfortunately, due to COVID- 19 pandemic the number of blood donors and consequently donated blood have dropped significantly. The lack is especially dire with regard to red blood cells and fresh frozen plasma (FFP).
Iwona Schymalla: In light of the situation you have just outlined, PPH prevention is becoming absolutely crucial. Is it feasible?
Maciej Socha: Definitely yes. We are supported by the body of knowledge and so able to determine the risk of PPH factors early on. Among them there is post CS condition of the patient, twin pregnancy, obesity or the patient's age. Taking into account these numerous PPH risk factors and the current situation it has never been more important to administer uterotonic drugs which contract the uterus. It is estimated that irregular and unstained contraction of uterus represents 50 to 70% of PPH. However, it needs to be stressed that we also have a significant number of patients without any PPH risk factors determined and still PPH occurs. Therefore it would be really important to implement pharmacological prevention that could replace widely-used oxytocin (now considered a standard). We have PPH preventive drugs already available on the market but their high price largely limits their wide-spread use.
Iwona Schymalla: So you would recommend a wide- spread PPH prevention and administration of the drugs, which are currently not reimbursed as I understand?
Maciej Socha: The issue is that both CS and vaginal delivery have comparable procedure estimation. If we can you use oxytocin and we use it in almost all cases as it significantly reduces the risk of PPH at the third stage of labor and moreover, is inexpensive. There are many studies which focus on the question of the second uterotonic drug to be used during labor to further reduce PPH risk. Unquestionably, this may help. However, administering another drug increases the risk of complications. Carbeticin, another form of oxytocin, commonly known as Pabal, a uterotonic drug we also administer, is capable of triggering sufficient contraction of uterus and simultaneously decreases the risk of using second uterotonic drug, which may result in higher rate of complications. This long-lasting drug appears to be the best option available.
Iwona Schymalla: What kind of educational support would HCPs need to receive with regard to the uterotonic drugs?
Maciej Socha: It seems that this support and awareness - raising are crucial. As I mentioned earlier PPH can lead to sudden deterioration of the patient's condition. That's why education really matters. The statistics confront us with brutal reality and indicate that administering appropriate preventive methods can decrease the risk of PPH, adverse side effects and death. And we are talking about deaths primarily caused by PPH. This long-lasting uterotonic drug is helpful in many ways e.g. there is no need to administer the second uterotonic drug in the next stages of labor and most importantly, it lowers the need of blood use. It enables us to decrease the blood loss by 80% – 500 to 1000ml , which is a lot, and in effect lowers the rate of complications and further impact, which is immensely important. We need to remember that the rate of CS is growing and currently stands at more than 40% of all deliveries. Moreover, in line with current recommendations, a patient diagnosed with COVID-19 should undergo CS. Such patients are prone to display a higher risk of complications. That's why carbetocin, a long-lasting formula, not oxytocin, is my first choice.
Iwon Schymalla: Let's hope that our patients will see this innovative treatment used in the near future.
Polska wersja materiału dostępna jest tutaj.