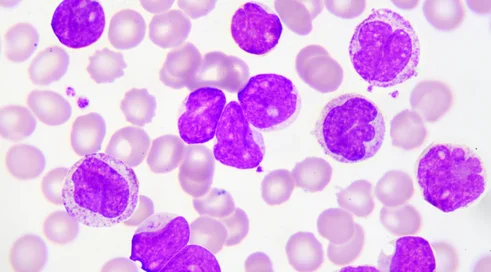
Prof. Krzysztof Giannopoulos: We still have unmet medical needs in plasmocytic myeloma

Published March 8, 2024 11:51

We recently celebrated Rare Disease Day, and all of March is Myeloma Awareness Month. I think it's a good opportunity to talk about what the priorities are when it comes to the needs in treating this disease.
Indeed, in plasmocytic myeloma, a great deal has changed in favor of reimbursement decisions of recent years. The decision at the beginning of this year, that is, to include daratumumab-lenalidomide-dexamethasone in the reimbursement program for a group of patients ineligible for transplantation, showed that in Poland we can treat very modern, according to international standards. I am talking here about first-line treatment. First-line treatment is currently a daratumumab-bortezomib-talidomide-dexamethasone regimen for patients eligible for transplantation. Later, we have the option of both consolidation therapy with the same regimen and, finally, the administration of maintenance treatment with lenalidomide, which is now a generic drug available in the benefits catalog.
The second, larger group of patients, comprising 70 percent of all plasmocytic myeloma patients, are those ineligible for transplantation. Here, the aforementioned availability of the most effective plasma cell myeloma therapy has come into play since January 1 of this year. The DRd regimen has shown tremendous efficacy, in fact there are no other therapies, even very modern ones, that are as effective. We pointed out during the reimbursement process that the transfer of daratumumab from the treatment of relapsed cases in the same therapeutic regimen has the benefit of extending the time to progression by an average of 20 months. This is a steep increase of up to one-third over the therapeutic results achieved to date.
Decisions about the first line of treatment will, of course, have consequences in later lines. The more effective we treat at the beginning, the more difficult it is for us to select therapy for recurrent patients. The first problem that will arise is the treatment of patients in the first relapse. As I said, basically all patients will receive treatment related to the use of lenalidomide. The big need is to secure adequate treatment for patients refractory to lenalidomide, which is a drug used for progression, regardless of dose, that is, both in the group of patients who are eligible for transplantation and receive lower doses in maintenance treatment, and in patients treated with lenalidomide regimens who are ineligible for transplantation. The efficacy of the regimens that are currently available in this group of patients will be limited, but we also have new registrations. Of note are triple-drug therapies, where the core of therapy is a carfilzomib-dexamethasone regimen. The same core of therapy is achievable in Poland and we are happy to use it, while it is achievable as a two-drug regimen. The addition of a third drug - a novel anti-CD38 monoclonal antibody, daratumumab or isatuximab - shows twice the efficacy, including in lenalidomide-resistant patients. This is where the first pressing reimbursement need arises, that is, reimbursement of the daratumumab-carfilzomib-dexamethasone regimen. This regimen is currently under consideration for reimbursement coverage. This is a very modern regimen, and it would be worthwhile for it to be available to Polish patients.
However, there will be problems after the third line of treatment, once we have used all the new drugs. In fact, international standards tell us that we should use immunotherapy, and here we have two therapeutic groups. One is CAR-T, already known to us for reimbursement in aggressive lymphoma or acute lymphoblastic leukemia. The situation here will be more complicated, because as of today none of the responsible parties has submitted a reimbursement application. Realistically, therefore, we cannot talk about CAR-T for the time being in terms of its availability in the treatment of patients with plasmocytic myeloma.
There is also a second group of immunotherapeutics. These are dual-specific antibodies, or antibodies that engage T lymphocytes. Three drugs are already registered. They are teclistamab, talvetamab and elranatamab. The first two are already in the reimbursement process, the first of which is at the most advanced stage. Here we have no choice, because there is no other therapy that can be used for these patients, meaning this is definitely an unmet medical need for plasmocytic myeloma patients.
Plasmocytic myeloma is a disease that meets the definition of a rare disease, but it seems that people with relapsed plasmocytic myeloma or lenalidomide resistance require a separate approach, as is the case in rare diseases. These are rare cases where we should really be able to have a comprehensive diagnosis and therapy.
Topics
szpiczak plazmocytowy