KDd regimen is the most urgent reimbursement need for second-line plasmocytic myeloma treatment

Published Dec. 21, 2023 15:00

From the beginning of the year, daratumumab, which was previously reimbursed in the dara-VTD regimen for patients eligible for transplantation now, will also be available in the daratumumab-lenalidomide-dexamethasone, or dRD, regimen for patients ineligible for transplantation. In practice, this means covering the entire population with a very modern, standards-compliant treatment.
- Such reimbursement decisions force the next ones to be made in a while, regarding reimbursement of regimens in subsequent lines of treatment. We can already see that a major challenge will be the patients who will receive lenalidomide in the first line," notes Professor Krzysztof Giannopoulos of the Department of Experimental Hematooncology at the Medical University of Lublin.
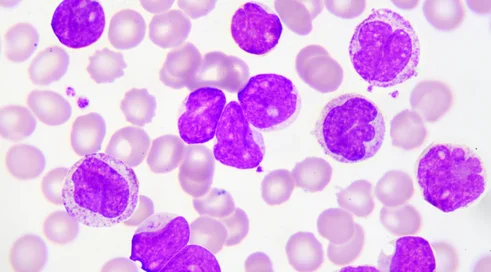
Lenalidomide is an oral immunomodulatory drug with high efficacy and taken continuously. It is well tolerated by most patients and is therefore taken until resistance, or treatment failure, occurs. According to hematooncologists, this is now the biggest challenge in terms of optimizing the treatment of relapsed patients.
- We know that this group of patients will not benefit from any therapy that has lenalidomide in its regimen. So the choice will be limited. Despite the reimbursement of various triple-drug therapies based on the lenalidomide-dexamethasone stem, they will not be able to be used," says Prof. Krzysztof Giannopoulos.
Hence arises the need to look for other schemes that could be used in the second line. Hematooncologists see two options. The first is regimens built on pomalidomide, a second-generation immunomodulatory drug. The second is regimens built on carfilzomib, a new-generation proteasome inhibitor, and dexamethasone.
- The studies we have show us the greater efficacy of three-drug regimens based on carfilzomib-dexamethasone. This seems to be the biggest reimbursement need right now. After all, we have a carfilzomib-dexamethasone (KD) regimen available for the treatment of relapsed patients, also with a convenient once-weekly dosing modification. However, with the results of studies comparing the efficacy of two-drug to three-drug regimens, we see an advantage for the latter. Both the combination with daratumumab and isoximab showed twice the efficacy as the KD regimen. What seems to be the greatest need is reimbursement for regimens in which the core of therapy is KD, but extended with a third drug. The reimbursement process for daratumumab is the most advanced. The KDd regimen would thus be the regimen of choice for the lenaldomide-resistant group, the professor believes.
The timeliness of reimbursement is important, he points out. The mentioned regimen uses daratumumab, an anti-CD38 antibody that is already starting to become a standard treatment for first-line patients.
- At the time of relapse, we would rather seek a different treatment than with daratumumab. The KDd regimen I'm referring to is best used in patients who have not received daratumumab, and there are many of them. This is the best treatment for patients resistant to lenalidomide," concludes Prof. Krzysztof Giannopoulos.