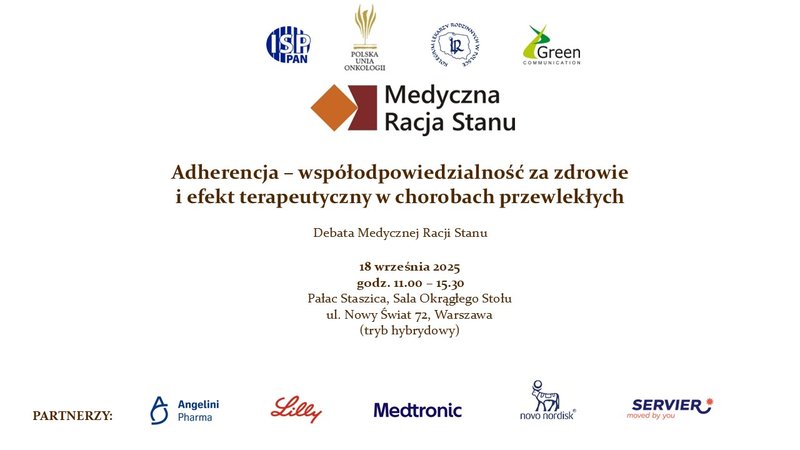
Adherence - shared responsibility for health and therapeutic effect in chronic diseases

Published Oct. 6, 2025 07:32

Non-adherence to therapeutic recommendations non-adherence is one of the most underestimated, and costly, health challenges in Europe. Therapeutic adherence, defined as the degree to which a patient adheres to recommendations for pharmacotherapy and other health interventions, is worth distinguishing from the term "compliance," which refers only to adherence to medical recommendations, especially taking medications. Adherence is a broader concept that also includes the patient's involvement in the treatment process, his motivation and awareness of the goal of therapy.
Adherence in the Diet
In May this year, a group of senators established the Parliamentary Adherence Team, which aims to create systemic solutions in connection with non-adherence to therapeutic recommendations. The work takes place in three sub-teams. The first deals with health education in the broadest sense, the second with the digital platform, accessibility to medical records, and the third with pharmacists. - In addition to issues related to the education of the medical community, from students to specialties, it is important to take advantage of the possibilities of digital medicine. Poland is becoming a leader in Europe in terms of e-prescribing. So we have excellent tools to monitor adherence. And it would be good if, with the patient's consent, medics could view all diagnoses and the medications they are currently taking with the ability to track prescriptions over the last year. We are also working to create tools that would supplement medical records with recorded voice, allowing more time for face-to-face conversations. And the third issue is the broader involvement of pharmacists. We have millions of visits a week to pharmacies and a huge potential when it comes to pharmacists' knowledge," said Professor Krzysztof Narkiewicz, head of the Department of Hypertension and Diabetology at the Medical University of Gdansk, who is cooperating with the Team. - The next meetings of the Team are already scheduled for early October this year. We hope that we will be able to complete some of the ambitious tasks we are carrying out already in the form of a pilot study by January next year," he announced.
Adherence in the aspect of mental disorders
Prof. Slawomir Murawiec, spokesman for the Polish Psychiatric Association, stressed that adherence is a central problem in psychiatry - We have many effective treatments, we know how to treat, while the central problem is lack of adherence. We struggle with patients' distrust of medications, psychiatrists and psychiatric hospitals, which is compounded by all sorts of perceptions," he explained. He added that new threats have emerged from the Internet, influencers and people who massively influence attitudes toward treatment. - Every six months or so, someone reports that medications either don't work, harm, or both, he pointed out.
Meanwhile, the problem of mental disorders is growing. Depression is a growing health problem, with NHF data showing that in 2023. 809,000 patients received services with a primary or comorbid diagnosis of depression. Reimbursed antidepressants used for depression, but also for other mental disorders, were purchased by 1.7 million people; if people buying non-reimbursed drugs are counted, it will be about 2 million. The number of hospitalizations for schizophrenia and the number of sick leaves issued for mental and behavioral disorders are increasing. In 2023, the Social Security Administration received almost 9% more such sick leave than in 2022. - The number of people who are struggling with mental problems is growing, and in younger generations, these are people struggling with not just one, but many at once - depression, anxiety, concentration disorders, attention disorders, eating disorders, relational problems and difficulties in processing information," enumerated Prof. Slawomir Murawiec.
Prof. Janusz Heitzman, president of the Polish Society of Forensic Psychiatry, also stressed that psychiatrists struggle with patients' non-acceptance of treatment, failure to recognize the dangers of the symptoms of the disease or sometimes even denying it. - The rate of intermittent treatment in mental disorders ranges from 40, almost to 60%, and is proportional to the ratio of mentally ill patients, who still face discrimination and stigmatization. And where discrimination and stigmatization is less, cooperation and adherence is better, he reported. He also pointed out the danger of loneliness for people with mental disorders, which also worsens adherence and often leads to excess hospitalizations sometimes in the absence of consent and the use of coercive measures. In such a situation, it is difficult to accept treatment. - So if a patient is already hospitalized, he or she must have recommendations to make cooperation in outpatient treatment more effective, more efficient and more acceptable, he pointed out.
Dr. Aleksandra Lewandowska, national consultant in child and adolescent psychiatry, stressed that it is also necessary to talk to a young patient about his or her disorder and conduct psychoeducation about the diagnosis itself. If a child or adolescent and his or her biscuits do not fully understand what the disorder entails, why pharmacotherapy and compliance with medical recommendations are important, such as in a diagnosis of schizophrenia or bipolar affective disorder, there is a high risk that medications will be used inconsistently, she explained. She stressed the role of cooperation between psychiatrists and psychologists and therapists, as well as communication with the school.
Dialogue with the patient
In a letter addressed to the participants in the debate, Minister Jolanta Sobierańska-Grenda addressed the topic of shared responsibility for health. - Each patient, doctor, pharmacist and the entire system must act together, be involved in creating a society for which health is the highest priority, she explained, pointing to the invaluable role of the primary care physician in the process of taking care of health. - He is the one who is in constant contact with the patient, monitors the course of therapy, reacts quickly to difficulties that arise and supports the patient in daily compliance with recommendations. Thanks to his involvement, patients feel safer, better understand the importance of therapy and are more cooperative, which translates into better health outcomes," the Health Minister emphasized in the letter.
Heading the Psychooncology Outpatient Clinic at the National Cancer Institute - PIB, Dr. Mariola Kosowicz spoke about patient education. - Working with patients has taught me humility, because even if something seems ideal to me for a patient, he or she may not have the knowledge resources to take care of his or her own well-being in this way, and not in another way. Also, you can't assume that if someone is educated, they have the ability to share responsibility for their health and life," she warned.
- If we want cooperation, both parties need to know what that cooperation is and what really needs to be done. For many people, the investment in health is important, yes, but it often seems to them that just going to the doctor decreases their responsibility and increases the doctor's. Cooperation is when we generate the possibility of co-medication, but such that the patient cares," said linguist Prof. Jerzy Bralczyk.
Prof. Artur Mamcarz advised to talk to the patient in the language of benefits. - It's not why we treat a patient to lower his blood pressure or cholesterol. It's to give the benefit of improving the quality of life, extending the duration of life in independence. Weight reduction is not a matter of fighting an aesthetic defect, but improving prognosis and prolonging life," he explained. He pointed out, however, that there is a group of patients to whom the language of loss appeals.
Tools to facilitate adherence in diabetes
Prof. Leszek Czupryniak, head of the Department of Internal Medicine Diabetology at WUM, stressed that a prerequisite for adherence in diabetes is to make the patient aware that treatment of a chronic disease means chronic medication. - Many people are convinced that if they get sick with something, they will take medication for a few days and it will pass. The best example of this is taking antibiotics. The professional group that takes antibiotics for the shortest time is doctors. On average, they stop treatment after three and a half days, which should last five or seven days, the expert reported. He added that there is also the other side of the coin. - The patient must be able to afford to take the drugs chronically. Even reimbursed GLP analogs are expensive," he pointed out. He added that patients will end up in the hospital every day because they have stopped taking their medications. - This is huge money, not counted at all in our country," he lamented.
Prof. Artur Mamcarz, head of the Department of Cardiology and Internal Medicine at WUM, pointed out that modern technologies improve adherence. - There is already evidence that glycemic monitoring systems without correcting therapy result in sugar leveling. Patients, seeing signals that something is wrong, correct the dietary pattern themselves, increase physical activity or respond to hypoglycemia, he enumerated.
Monika Kaczmarek, president of the Polish Diabetes Association, pointed out that every patient has reimbursement for insulin pumps until the age of 26, but after that it is taken away from them. - The patient loses his sense of security, which is often associated with depression, and his therapeutic process regresses, she recounted. - Further reimbursement would definitely help keep the patient on therapeutic recommendations and at the same time balanced diabetes, she urged. She also talked about an educational project implemented by the Polish Diabetes Association among patients who have not had and do not have reimbursement for continuous glycemic monitoring systems. - Thanks to these systems, their awareness of their own disease in the first place improved, but also their knowledge of how to act, the impact of nutrition, physical activity and stress. Patients adhered better to therapeutic recommendations because they could see the effects," she pointed out.
Adherence in the treatment of obesity
Ewa Godlewska, president of FLO - Foundation for the Treatment of Obesity, stressed that obese patients are still stigmatized and discriminated against, both in society, in the family environment, and ¾ of them in doctors' offices. She reported that of the 9 million adults suffering from obesity in Poland, about 2% are treated. By the time patients get to the doctor, they have had several or more attempts to treat their obesity disease unsuccessfully. - In order for the patient to take up treatment and persevere, it is necessary to have effective inclusive communication with the doctor, not to judge the patient, who blames himself all his life anyway, that he is weak, that he has no strong willpower, that he overeats," she pointed out. She added that the important thing is to explain what bariatric surgery, drug treatment and lifestyle changes that coexist with both types of treatment entail.
- If the patient does not know what the role of the drugs used to treat obesity is, they will treat them as a panacea for weight loss and when they fail to reduce weight, the therapy will be abandoned, she explained.
She lamented that pharmacotherapy is unreimbursed and treatment is expensive. - Today in Poland, obese patients have access neither to reimbursed drugs nor to a therapeutic team that can support them in the treatment process. This is the only group of patients who are really left to their own devices," she said.
Dr. Maria Humięcka of the CMKP Department of Internal Medicine and Gerontocardiology also lamented that GLP analogs are not reimbursed for the treatment of obesity. - Patients often want to learn more about these drugs, they ask the doctor about their mechanism of action, how long the treatment lasts, and this creates space to explain to them that although the drug reduces appetite, it is up to the patient's decision how much food to take in, she pointed out.
Prof. Piotr Jankowski, head of the Clinical Department of Internal Medicine and Gerontocardiology at the Witold Orlowski Independent Public Clinical Hospital, stressed that studies have shown that bariatric surgery is effective when accompanied by lifestyle education, modification of daily behavior, dietary choices, physical activity and, if indicated, pharmacotherapy.
He stressed that surgical treatment of obesity reduces cardiovascular risk, is an effective treatment for hypertension, diabetes, lipidemia. It causes remission of these diseases. - After 10 years, in many patients who had hypertension, diabetes, elevated cholesterol before surgery, it has been possible to reduce the number of drugs, reduce their doses, and in some patients to discontinue pharmacotherapy, he stressed.
Prof. Mariusz Wyleżoł, president-elect of the Polish Obesity Society and head of the Warsaw Obesity Treatment and Bariatric Surgery Center at Czerniakowski Hospital, said that his hospital is implementing a program for comprehensive treatment of obese patients in a friendly environment. - This is because there are still few people who understand that this is a disease that the patient does not choose for himself, which can develop like any other, which devastates life and health, and before it leads to death causes exclusion and disability, he pointed out.