Oxygen Increased Flow Advanced Membrane heralds a new era in the treatment of patients with severe cardiopulmonary failure. The project's developers hope that the successor to extracorporeal membrane blood oxygenation, ECMO, has just arrived. In the 6th Start-Up-Med Competition, which was a side event of the recently concluded 9th Health Challenges Congress in Katowice, the Silesian Medical University in Katowice won in the medical/scientific center category, having just presented the OXIFlame project.
What is ECMO?
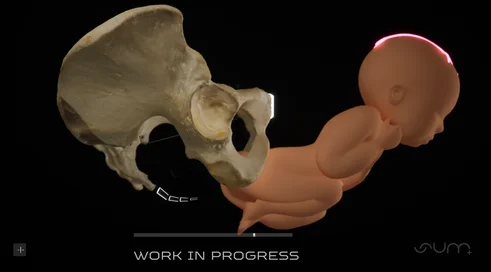
Extracorporeal membrane oxygenation (ECMO, or extracorporeal membrane oxygenation) is a technique that involves oxygenating (oxygenating) the blood and eliminating carbon dioxide from it in an oxygenator, using extracorporeal circulation.
ECMO is used only in patients, in potentially reversible life-threatening conditions with very severe respiratory and/or circulatory failure, who have failed to respond to conventional treatments available in intensive care units.
ECMO does not cure the heart or lungs, but gives the patient a chance to survive the period when these organs are failing. It gives the doctor time to treat the disease that led to extreme cardiopulmonary failure.
There are two basic schemes for connecting veno-venous ECMO veno-venous (veno-venous VV ECMO) is used as respiratory support, while veno-arterial (veno - arterial VA ECMO) is used as cardiac and/or respiratory support.
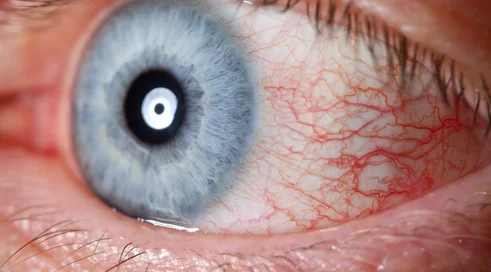
VV ECMO is used in patients with severe acute respiratory distress syndrome (ARDS), in which the so-called alveolar-capillary barrier is damaged, causing protein-rich fluid to leak into the respiratory system. The collapse of the alveoli causes the lungs to lose their ability to perform their function of exchanging oxygen and carbon dioxide, leading to hypoxia (anoxia). Among...
Content locked
To gain access to the complete English section of the Medexpress.pl, kindly reach out to us at [email protected].