There are ESMO guidelines for the treatment of thrombosis in cancer patients

Published March 23, 2023 11:50

.
Medexpress: Thromboembolic incidents - how significant is this problem in cancer patients?
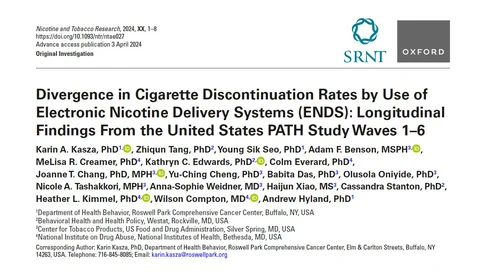
L.W.: This is a problem that has long been known to be important. As early as the 19th century, syndromes associated with thromboembolic disorders in cancer patients were described. Since then, our knowledge has expanded greatly. Medications have long since appeared, which we use both for prevention and treatment. Today we are talking because there are new recommendations from the European Society of Clinical Oncology (ESMO) for the management of these conditions. And this is very important, because the ESMO recommendations raise the profile of the problem of thromboembolic disorders in oncology.
Medexpress: What do the new ESMO recommendations bring?
L.W.: We have such a tendency now that various other fields of medicine are being tacked onto the word "oncology" - so we have, for example, cardiooncology. On the one hand, ESMO, seeing this, is eager to cooperate with cardiooncology societies, trying to reach oncologists in a simpler way, showing them what the management should be, that it should be comprehensive and the patient should receive full oncological care, including for diseases accompanying cancer. The new recommendations themselves more systematize the results of studies on the diagnosis and treatment of thrombotic disorders in oncology. Their important role is that they assign scientific value to individual reports, which even results in an obligation on the part of physicians to follow the recommended procedures if they treat oncology patients.
Medexpress: What are the specifics of these recommendations? How should and hopefully will clotting disorders be treated in cancer patients in Poland now?
L.W.: The big breakthroughs in these recommendations are not there. There is an emphasis on the role of postoperative prophylaxis of thrombotic disorders in cancer patients. And here we always have a division between patients with high and low risk of postoperative bleeding (prophylaxis reduces the risk of thromboembolic disorders, but on the other hand increases the risk of bleeding). Admittedly, to a greater extent, it reduces our risk of thromboembolic disorders by an average of five times, but only increases the risk of bleeding by 2.5 times. But if a particular procedure has an individual higher risk of bleeding, it is clear that anticoagulants must be used with some caution. We also have an emphasis on the role of mechanical prophylaxis in preventing lower extremity thrombosis. Another important element is to determine the risk of individual thrombotic complications in a particular patient, related to immobilization, malnutrition or the type of cancer. And here ESMO provides the appropriate risk scales. If a patient has a defined high risk of such complications of 8-10 percent, then we have an indication for prophylaxis, in parallel with the start of oncological treatment.
We have specific recommendations for increased prophylaxis in pancreatic cancer patients. And we also have what the patient community has been waiting for, which is to elevate the role of oral medications in the prevention of thromboembolic disorders. This is an interesting option. She is safe. Oncologists are not afraid of this. However, it is not directly related to the registration provisions with these preparations. And this causes some limitation in the reimbursement of anticoagulants. It is not my purpose here to pronounce whether this reimbursement should take place. The important thing is that the patient, in accordance with the code of medical ethics, should be informed that there are certain data that speak about the possible use of such preparations. Some oncology patients express a certain aversion to additional medical procedures, such as giving themselves injections. And here, especially in patients who are active, this reluctance is high. And meanwhile, even full-price drugs in this group are not so unimaginably expensive that some patients choose not to take them. However, oral pills instead of 30 or 60 injections a month make a big difference in quality of life, and it is eminently important in palliative treatment.
You can read the text of the ESMO guidelines here.